Pelvic Pain: Your Questions Answered
If you’ve been here a while I hope you’re starting to love the pelvis as much as I do. If you’re new - welcome!! We’re always excited to add to our community.
On March 7th, 2021 I had the pleasure of presenting a topic in women’s health alongside a group of amazing women practitioners to celebrate International Women’s Day. I chose to speak about pelvic pain because I think we all deserve to be comfortable and confident when speaking about pelvic health. That comfort and confidence comes in part from knowing the anatomy, symptoms, and treatment options available to you.
Do you have pain in the hips, thighs or below your low back when walking for long periods of time?
Are you pregnant and you have pain in your pelvis that you haven’t experienced before?
Have you recently had a baby (postpartum or postnatal) and you are continuing to experience pelvic pain?
Are you wondering the different options for managing or treating pelvic pain?
These are some of the most commonly googled questions when looking up “pelvic pain.” If you’ve had these questions before, this post is for you!
First, some anatomy:
It’s really hard to talk about the ins and outs of pelvic pain and other pelvic health concerns without discussing the anatomy of the pelvis.
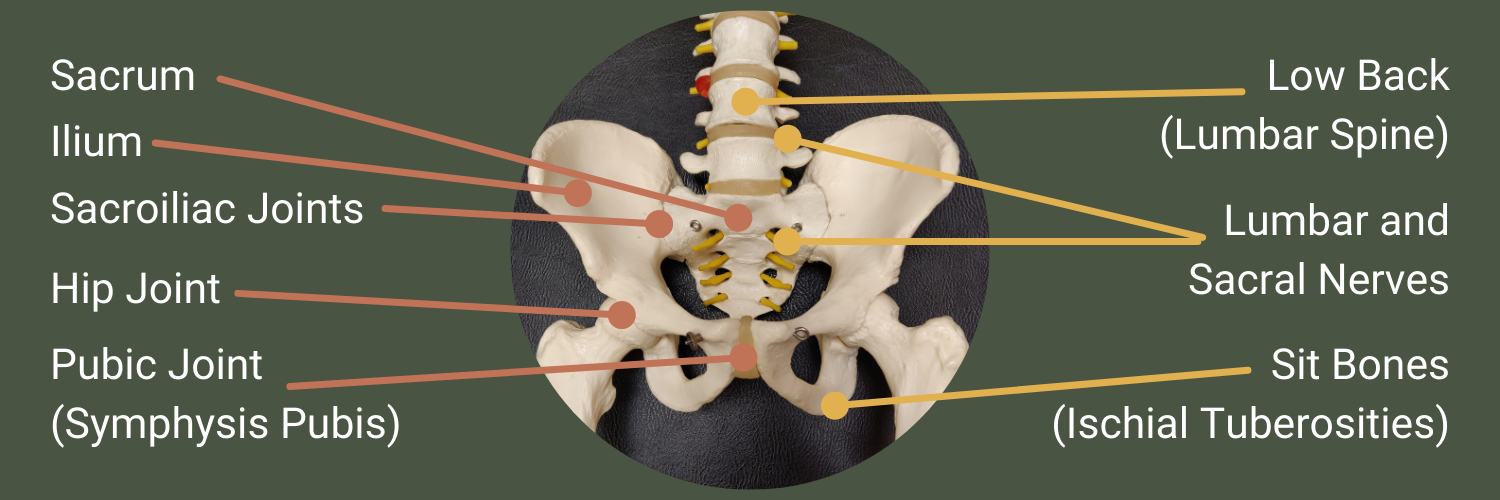
Bones and Joints of the Pelvis
The sacrum is the bone found at the base of the spine. If you can locate the two “dimples” between the back and the buttocks, then move towards the midline from there, you can feel your sacrum.
The tailbone or coccyx is not seen in the image, but it is located at the very bottom of the sacrum.
The ilium is the “wing,” or upper half of the pelvis.
The sacrum and ilium attach together to form two very strong, robust joints with very little motion, called the “sacroiliac joints”. These joints allow weight transfer between the lower body and the upper body with every day movements.
While not truly a joint in the pelvis itself, the hip joints are ball and socket joints between the thigh bone (femur) and the pelvis. Sometimes pain in the pelvis can refer or travel to the hip or vice versa, so it’s worth mentioning here.
If you locate your belly button and travel downwards until you hit a bony area, that is your pubic joint, or symphysis pubis. This is another very strong, robust joint that helps to transfer weight between the lower and upper body. Around the pubic joint is attachment sites for the groin, or adductor muscles.
The low back or lumbar spine is not part of the pelvis, but it is where your pelvis attaches to the spine via the sacrum.
Between each bone of the spine, and coming out from small holes in the sacrum, are pairs of lumbar and sacral nerves. These provide sensation, motion, and other types of innervation to the lower limbs and pelvis.
Also called ischial tuberosities, the sit bones are the supportive anatomy for when you sit. They are important attachment sites for the hamstring muscles on the back of the legs.
Source (muscle images): Beth ohara (raster), Offnfopt (vector), CC BY-SA 3.0 <https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons
Muscles of the Core and Pelvis
The “inner core” or “deep core” is shaped somewhat like a cylinder, with four muscles working together to provide breath, stability, and support during daily activities and exercise.
The diaphragm is the muscle that helps you breathe. It is located under the lungs, and moves downward to allow air into the lungs as you inhale.
The pelvic floor is in the bottom of the pelvis. It is a group of muscles and other soft tissues that support the pelvic organs. As you inhale and the diaphragm moves downwards, your pelvic floor also moves downwards to allow space for the abdominal contents.
The multifidus is a set of muscles that attach between each vertebrae, or each bone of the spine, providing support, stability, and feedback to your brain about where your body is in space.
The transversus abdominis is a corset-shaped muscle that wraps around your abdomen, again providing support and stability. It turns on automatically in response to load and movement.
While there are many muscles in the pelvis, the largest ones, and ones most relevant to a general understanding of pelvic pain are the gluteus maximus, gluteus medius, and piriformis muscles.
The gluteus maximus, or “glute max,” extends the leg at the hip. For example, when you are walking and one leg is behind you, your glute max activated to pull your thigh bone backwards.
The gluteus medius, or “glute med” is an important muscle for stabilizing the pelvis when you perform asymmetrical, one-legged, or any activity where force is not equal through both of your lower limbs.
The piriformis externally rotates the hip when in neutral standing position.
Who gets pelvic pain?
Pelvic pain can happen to anyone, but it is more common:
during pregnancy
postpartum (postnatally)
in persons with certain types of arthritis
in persons who have experienced a major trauma to the pelvis
there is also a subset of the fitness community who participate in high impact activities that experience pelvic symptoms, especially urinary symptoms such as leaking
Can men get pelvic pain?
Yes, men can also get pelvic pain and other pelvic symptoms. The muscles and joints of the pelvis are similar between all genders. There are also conditions more common in men, such as prostate trouble, which may contribute to pelvic pain and other symptoms.
What are some symptoms of pelvic pain?
Depending on the cause of your pelvic pain you may experience differing symptoms. These symptoms are more commonly related to a specific condition called pelvic girdle pain.
Pain:
near or at the sacroiliac joints
near or at the pubic joint
near or at the tailbone
that sometimes catches you off guard
travelling around the sides of the hips
travelling down the inner thighs
when walking, sitting, or lying down for long periods of time
when putting on pants or socks one leg or foot at a time
Other symptoms:
pain in the pelvic floor, or the base of the pelvis in the area between the legs
urinary symptoms including incontinence (leaking), burning, or pain
pain during penetrative sex
I am experiencing pain in my pelvic floor.
I am experiencing pain during sex.
I am experiencing urinary changes (burning, leaking, pain).
What should I do?
Firstly, there are options for you! I highly highly recommend you speak with a trusted healthcare provider. If your complaint has not been addressed by your current provider it doesn’t hurt to speak to someone else. Speaking with a physiotherapist with additional training in pelvic health is a great place to start (also called a pelvic floor physiotherapist). If you’re being seen in clinic by your chiropractor, please let them know you’re experiencing pelvic pain during sex. As part if your healthcare team they want to know about symptoms that bother you, and they might be able to provide some general advice until you can have the issue addressed by someone who performs internal exams, or they might be able to find you a referral to another professional.
Is there a difference between low back pain and pelvic pain?
While some of the symptoms listed above may sound similar to low back pain, and sometimes pelvic pain is wrapped up into the package of non-specific low back pain, there are some differences between the two conditions, especially when diagnosing and managing them.
Pain in the low back:
Location: above the back “dimples” and below the rib cage
Travel: possibly down the back of the leg(s) (most commonly)
Positions of Aggravation: often either flexion or extension postures
Relieving Factors: activity or sleep/laying down
Compared to pelvic pain:
Location: top of the hips to the gluteal fold (the bottom of the cheeks of the buttocks), including the pubic joint
Travel: around the hips, down the inner thighs (most commonly)
Positions of Aggravation: “asymmetrical” positions such as walking, putting on pants, standing on one leg, etc. Even laying down may be painful.
Relieving Factors: using both legs or hips at the same time, with the same load through each leg
Importantly, you can have both the low back and pelvis generating pain at the same time, so seeing a skilled clinician that can determine where your pain is coming from is important!
What causes pelvic pain?
Short answer: there are many possible contributors to pelvic pain, and with certain types of pelvic pain we don’t have a definitive answer. That said, let’s look at some of the things assess in clinic:
A change in biomechanics? There are many things that can contribute to altered biomechanics, including changes in spinal curvature during pregnancy, pre-existing pain changing how we move our joints and muscles, or repetitive strain on tissues during suboptimal postures and positions. Although we do not have good evidence that changes in posture and spinal curves contributes to pelvic pain, postural changes can be quickly and easily addressed with minimal side effects and low cost, so they are a good option for some people to pursue.
A change in hormones? At one time it was thought that increased joint laxity caused by pregnancy-related hormones contributed to pelvic pain. More recent evidence however does not support that idea. This is not to say that pregnancy-related hormones do not contribute to other musculoskeletal conditions, just that they do not seem to be an important factor in pregnancy-related pelvic girdle pain.
A change in muscle balance and force? The sacroiliac joints are strengthened through “form” and “force” closure. The articulating, or attaching, surfaces of the ilia and sacrum are very rough, and conform to each other well, which creates a lot of friction. This is what creates “form closure.” The large muscles and other soft tissues in the area that cross the joints create a lot of force across the joint, increasing the friction and the articulation of the joint itself, contributing to “force closure”. Sometimes one of these elements, more commonly force closure, is altered and the body interprets the new imbalance as pain, creating the sensations listed above.
A change in the pelvic floor tone? Pain and urinary changes may be a symptom of too little or too much tone in the pelvic floor. Many people are familiar with kegels or pelvic floor contractions with the goal of strengthening or increasing the tone of the pelvic floor, but these exercises focusing on increasing tone are not right for everyone. In people with pelvic pain, too much tone can be a culprit.
What are some treatments for pelvic pain?
Treatments for pelvic pain generally are “conservative” in nature, meaning most people do not require major medical intervention or surgery. That being said, the treatment option that is best for you is best discussed with a health professional.
Speak to a Healthcare Provider
First, if you’re experiencing pelvic pain, especially new pain, it is best to discuss your concerns with a trusted healthcare provider. I often reference chiropractors and pelvic floor physiotherapy as I am a chiropractor and I work closely with pelvic floor physios. As a chiropractor, in clinic I use a combination of:
personalized advice on ways you can manage the activities that bother you
manual therapy, or hands on care, including adjustments, soft tissue therapy, or joint mobilization
personalized exercises with advice on how to safely and correctly perform exercises
To help my patients manage pelvic pain.
Posture Modification
Something you can try at home is modification of your sitting, standing, or laying down postures.
For example, try sitting with the hips abducted and externally rotated. Another way of saying this is to try sitting with the knees apart instead of close together, and the hips rotated outwards. Some examples are shown in the image to the right (desktop) or above (mobile). This posture helps increase force closure of the sacroiliac joints, as discussed above.
Abdominal Breathing
In addition, I often recommend practice in abdominal or diaphragmatic breathing with spinal or pelvic pain. Abdominal breathing can help to restore coordination or bring awareness to the core muscles, and it can help activate the parasympathetic or “rest and digest” element of the nervous system.
Take three breaths and notice what you feel.
Did you feel tightness, discomfort, fullness, relaxation, anywhere on your body?Think about your pelvic posture. If you’re sitting back against your sacrum with your spine rounded, try tilting your pelvis until you’re sitting on your sit bones. Take three more breaths.
Did anything change?Finally, place one hand on your belly and another on your chest. Bring awareness to how much air is moving in your belly, and which hand moves first. If the chest moves first or moves a lot more than the belly, try to allow your breath to fill the belly.
[This abdominal breath will be a future topic on my Instagram - once I’ve created the post I’ll upload it here!]
Can I use a belt for pelvic pain?
The American Physical Therapy Association guideline lists a support belt as a potential option for managing pelvic girdle pain. It would be worthwhile to see a practitioner that can help you decide if a support belt would be right for you, as fitting and wearing the belt correctly are important for comfort, and possibly important for how well the belt works. Further, while a support belt might help some people, they are only a temporary solution and there are other treatment options that may be better suited to you for longer-term care.
What are some exercises for pelvic pain?
It is important to know that there are exercises that you can perform to strengthen weakened or inhibited muscles, and releases to relax overactivated muscles in your core or pelvis. These are discussions best had with your healthcare provider as some exercises may be helpful for some types of pelvic pain, and exacerbate the condition for other types of pelvic pain.
A good starting point, however, is to maintain your general daily activity. If you enjoy walking, continue walking. Sometimes people with pelvic pain will change how they walk to try to reduce the pain, but if possible try to walk without those changes to your gait.
What are my next steps?
First I hope you’ve learned a little about your pelvis! If you’re experiencing pain, perhaps:
Book an appointment with your chiropractor or physiotherapist. If you’re looking for a chiropractor, my booking site is brucevillage.janeapp.com, or I have a direct link at the “Make an Appointment” button below and at the top of the page. I would love to meet you!
Use as much anatomy and terminology as you’re comfortable using while describing your complaint to your healthcare provider. If there’s something that concerns you, please bring it up, nothing is off limits. We’ve heard it all, there is no topic that we’re not comfortable discussing!
In the mean time, maybe try some of the things listed above, and think about how they change your symptoms. This can be valuable information for you or your care provider.
References:
Clinton SC, Newell A, Downey PA, Ferreira K. Pelvic girdle pain in the antepartum population: Physical therapy clinical practice guidelines linked to the international classification of functioning, disability, and health from the Section on Women’s Health and the Orthopaedic Section of the American Physical Therapy Association. J Women’s Health Physical Ther. 2017 May/Aug [cited 2020 Apr 8]; 41(2):102-125.
Faubion SS, Shuster LT, Bharucha AE. Recognition and management of nonrelaxing pelvic floor dysfunction. Mayo Clinic Proc. 2012 [cited 2021 Mar 17]; 87(2):187-193.
Mottola MF, Davenport MH, Ruchat SM, Davies GA, Poitras VJ et al. 2019 guideline for physical activity throughout pregnancy. J Obstet Gynaecol Can. 2018 [cited 2020 Apr 8]; 40(11):1549-1559.
Rost C, Britnell S. Rost Therapy: Evidence-Based Management of Pregnancy-Related Pelvic Girdle Pain [Course Online]. 2018 [cited 2020 Apr 8]. Available from: www.rosttherapy.com.
Stuber KJ, Wynd S, Weis CA. Adverse events from spinal manipulation in the pregnant and postpartum periods: a critical review of the literature. Chiropractic and Man Ther. 2012 [cited 2020 Apr 8]; 20:8-15.
Vleeming A, Albert HB, Ostgaard HC, Suresson B, Stuge B. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J. 2008 [cited 2020 Apr 8]; 17(6):794-819.
Vopni K. Core Confidence and Pre/Postnatal Fitness Specialist Certification [Course Online]. 2019. Available from: www.vaginacoach.com.
Weis CA, Barrett J, Tavares P, Draper C, Ngo K, Leung J, Huynh T, Landsman V. Prevalence of low back pain, pelvic girdle pain, and combination pain in a pregnant Ontario population. J Obstet Gynaecol Can. 2018 [cited 2020 Apr 8]; 40(8):1038-1043.